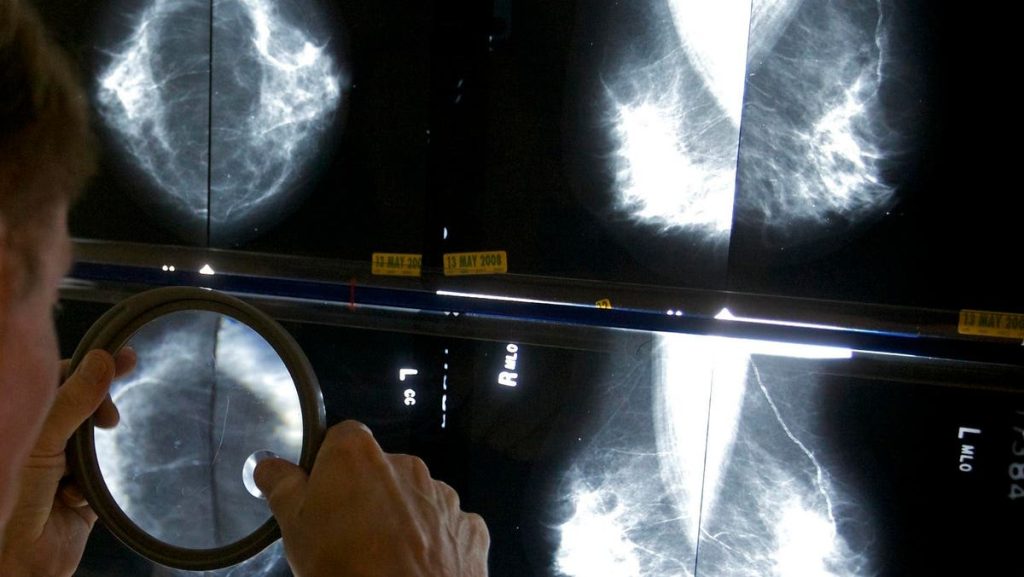
Can artificial intelligence (AI) help detect breast cancer? A new study out of Sweden has tentatively said: yes.
The study enrolled over 80,000 women in a clinical trial to ask this question. All 80,033 underwent mammography. Half of those mammograms were interpreted the standard way in Sweden, which is by two physicians. The other half had their mammograms read by a physician (or two physicians) who had an AI-supported analysis.
What’s an “AI-supported analysis?” That’s when the AI system reviewed the images of the mammogram first, then gave the images a score from 0-10. The image and the score then was reviewed by a radiologist (or two radiologists if the score was 10, the highest risk score).
What we know
The study found that AI-supported screening found 20% more cancers as compared to the standard review by physicians who did not use AI.
AI-supported screening did not increase the number of false positives, meaning it did incorrectly diagnose mammograms as abnormal.
The workload of radiologists was reduced by 44% when using AI. However, an important difference between the US and Sweden is: in the US, mammograms are only read by one physician, not two. So the benefit of saving time is, at baseline, less important in the US as compared to Sweden.
What we don’t know
We don’t know the final results of the study, which will take two years (this analysis was done after one year). Interim analysis are exciting and interesting, but they are not the final results, so stayed tuned for updates about this study.
“These promising interim safety results should be used to inform new trials and program-based evaluations to address the pronounced radiologist shortage in many countries. But they are not enough on their own to confirm that AI is ready to be implemented in mammography screening,” cautions lead author Dr Kristina Lång from Lund University, Sweden, who spoke to The Lancet. “We still need to understand the implications on patients’ outcomes, especially whether combining radiologists’ expertise with AI can help detect interval cancers that are often missed by traditional screening, as well as the cost-effectiveness of the technology.”
Dr. Laurie Margolies MD, vice chair of breast imaging at the Icahn School of Medicine at Mount Sinai, NY, shared: “We have seen some women with a low AI score, turn out to have concerning findings diagnosed by the radiologist. AI is an important and helpful tool but it’s not a replacement for the physician’s review.” For example, AI can miss breast lymphoma, which looks very different from a typical breast cancer on a mammogram.
The future of AI for breast screening
Dr. Margolies says that AI is already being adopted in the U.S. and will continue to be utilized more frequently in the future, because it helps expedite decision making. It also can hopefully lower the recall rate, i.e. which is the rate at which women who are called back for more imaging if their first mammogram is equivocal. The current recall rate in the U.S is 5-12%, which is much higher than the 2% in the Swedish study. Lowering the recall rate is important because “it saves patients the anxiety of having to come back for another exam and it lowers healthcare costs,” says Dr. Margolies.
Another potential benefit of AI-assisted mammography include risk stratification, especially for women with dense breasts that may have subtle patterns that AI can help identify and track over time. In addition, Dr. Margolies believes that breast arterial calcifications are a developing field of medicine and may help identify women with heart disease. While the goal of mammograms are to detect breast cancer, there are arteries in the breast that, if calcified, could represent heart disease. AI could potentially help find these abnormalities that are often not diagnosed elsewhere.
In sum, use of AI-assisted mammography holds a lot of promise and its adoption will likely continue as physicians find new ways to use this exciting tool.
Read the full article here