Topline
Officials in Thailand on Wednesday said they have detected a new case of mpox in the country and are investigating to see whether the variant is the same linked to a growing outbreak in central Africa, as the World Health Organization urges nations to come together and tackle the virus days after it sounded the alarm over a dangerous new variant driving a worrying outbreak of the disease in central Africa
Timeline
Thailand detected an mpox case in a European tourist arriving from Africa last week and health officials said they are treating it as if it is the newer clade I form of mpox while awaiting test results to ascertain the strain, with the results expected in a few days.
“We can and must tackle mpox together,” WHO regional director for Europe Hans Kluge told reporters, urging nations to “control and eliminate mpox globally” with well-known strategies available to us rather than “enter another cycle of panic and neglect.”
The Philippines reported its first case of mpox this year in a 33-year-old man with no history of travel outside the country, the Department of Health said, later adding that the case is not the same form as the newer clade I variant driving a growing outbreak in Africa but the milder clade 2 variant.
Pakistan confirmed at least one case of mpox in a patient returning from an unspecified Gulf country—reports have named both Saudi Arabia and the United Arab Emirates (UAE)—though testing later revealed it was not the new clade Ib strain but the distinct clade II variety.
Sweden became the first country outside of Africa to report an mpox infection caused by the clade I variant, though officials said the person had been infected during a stay in the region and stressed the risk to the general population from the virus is “very low.”
The World Health Organization declared the mpox outbreak a public health emergency of international concern, the agency’s highest level of alert under international law.
At least 12 countries in Africa have reported mpox outbreaks so far, the Africa Centers for Disease Control and Prevention (Africa CDC) said when declaring an emergency, including four—Burundi, Kenya, Rwanda and Uganda—that have not reported mpox before.
The vast majority of cases have been reported in the Democratic Republic of Congo (DRC), the historic confines of the variant for more than a decade, and at least 12 nearby countries, including those listed above, have confirmed cases or are considered to be at high risk due to sharing a border with the DRC: Republic of the Congo, Central African Republic, Rwanda, Cameroon, Gabon, Angola, South Sudan, Tanzania and Zambia.
Crucial Quote
“We encourage all countries to enhance surveillance, share data, and work to better understand the transmission; share tools like vaccines; and apply lessons learned from prior public health emergencies of international concern in addressing the current outbreak,” WHO chief Tedros Adhanom Ghebreyesus said.
How Many Cases Have Been Reported?
African officials have confirmed 2,863 mpox cases and 517 deaths in 2024 so far, according to Africa CDC, most in the DRC. Only a fraction of suspected infections are genetically tested to confirm mpox and determine the variant responsible and officials said the number of suspected cases have already surpassed 17,000, vastly exceeding last year’s total around 15,600 cases and 537 deaths. These figures are “just the tip of the iceberg, experts said, due to difficulties with tracking and testing cases.
What Is Mpox?
Mpox, formerly known as monkeypox, is a viral illness caused by infection with the monkeypox virus. The virus belongs to a large family of viruses known to cause disease in humans and other animals, including smallpox, or variola, cowpox, Alaskapox, and vaccinia, a weakened form of which is used in mpox and smallpox vaccines. Mpox infections are typically mild but infections can and do kill, with data suggesting the clade I variant has a death rate as high as 10%. Young children, pregnant people and those with compromised immune systems are most at risk of poor outcomes. Symptoms of infection include a fever, swollen lymph nodes and characteristic, pus-filled rash and the virus spreads primarily through close contact with infected people, animals or contaminated materials like towels.
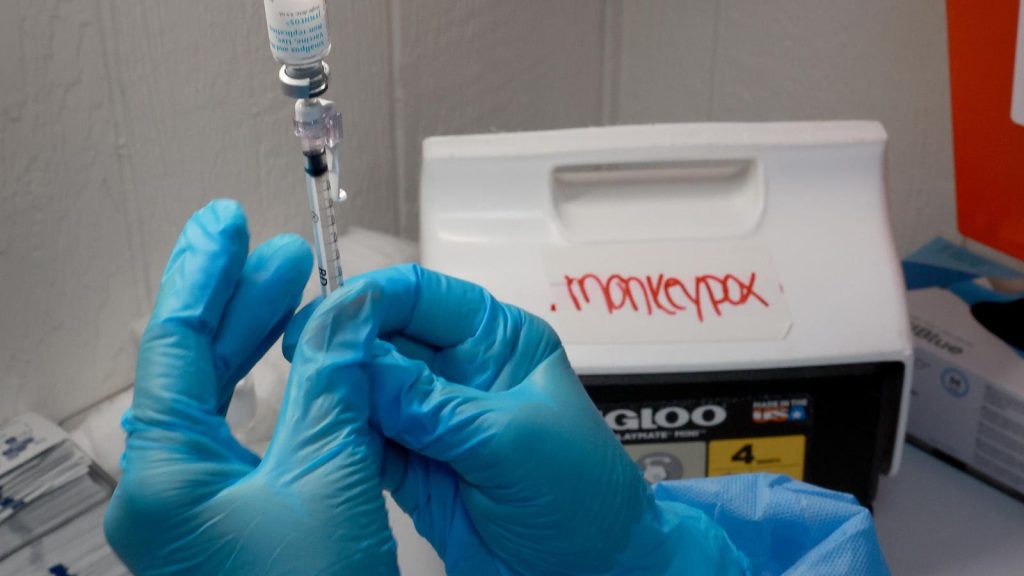
Are There Mpox Vaccines?
Yes. The preferred choice among health officials is Bavarian Nordic’s two-dose vaccine. The shot, sold as Jynneos, Imvamune and Imvanex, has a more favorable risk profile to available alternatives and has been authorized for use against mpox by major health agencies around the world, including the Food and Drug Administration. The company says it can supply 10 million shots to combat the outbreak by the end of 2025, with 2 million by the end of the year. There are plentiful stores of Emergent BioSolutions’ smallpox vaccine ACAM2000 in national stockpiles around the world. The shot, kept for national security in case the now-eradicated smallpox somehow resurfaces or is deployed as a weapon, is not generally favored for widespread use due to its higher risk of potentially serious side effects but could be turned to protect against mpox if needed. KM Biologics secured approval for its smallpox and mpox vaccine, LC16, in its home country of Japan during the 2022 outbreak. But the company has not sought widespread approval for the shot around the world and it is not commercially available. There are reportedly significant supplies in Japan’s national stockpile should Tokyo release them. Another smallpox vaccine that could be turned against mpox has also been approved in Russia. The shot, which the WHO says is the “first fourth-generation smallpox/orthopoxvirus vaccine,” is not widely available, however, and given the agency that developed it, it is not known whether Moscow would share supplies internationally. The shot was developed and registered by Russia’s Vector institute, the historic home of the Soviet Union’s biological weapons program and host to one of two authorized smallpox repositories globally (the other being the CDC).
Who Should Get Vaccinated Against Mpox?
Most countries consider the risk of an mpox outbreak to be very low and have not endorsed widespread vaccination. The Centers for Disease Control and Prevention recommends mpox vaccination in the U.S. for the at-risk groups identified during the last global outbreak in 2022 and while cases have fallen, the virus variant still circulates. This includes gay, bisexual or other men who have sex with men or transgender, nonbinary or gender-diverse people, particularly those who have multiple sex partners, have sex at commercial sex venues like clubs or saunas and have received a new diagnosis of a sexually transmitted infection like chlamydia, gonorrhea or syphilis in the last six months. People with an occupational risk of exposure such as laboratory or healthcare workers are also recommended to get the shot, as are people who have had sex with or been exposed to someone diagnosed with mpox. The agency recommends two doses of Jynneos administered four weeks apart.
What Happened To The Other Mpox Variant?
The clade II variant that drove the 2022 mpox outbreak is still circulating. Cases in Western countries have dwindled following widespread vaccination efforts but cases still crop up and officials monitor the virus’ movements closely. The variant is also still responsible for outbreaks in Africa, predominantly western Africa, where it has historically circulated. When reporting on the clade I outbreak, the WHO noted a “separate” mpox outbreak in the Côte d’Ivoire linked to clade II.
Get Forbes Breaking News Text Alerts: We’re launching text message alerts so you’ll always know the biggest stories shaping the day’s headlines. Text “Alerts” to (201) 335-0739 or sign up here.
Read the full article here