Topline
Ozempic and Wegovy manufacturer announced it will take legal action against facilities illegally compounding the drugs amid persistent shortages, which have left some patients without medication.
Key Facts
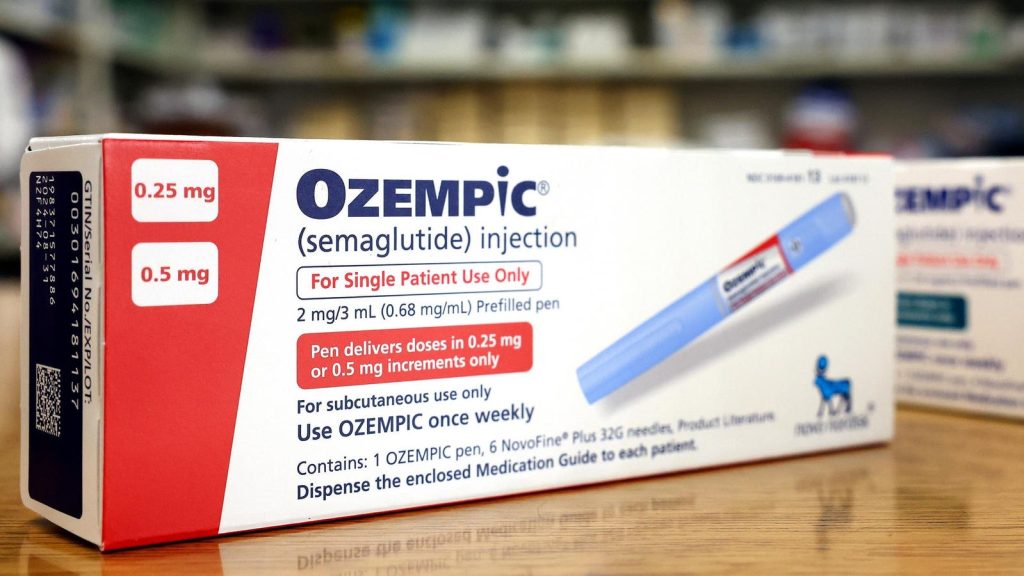
Novo Nordisk, the maker of Ozempic, Wegovy and Rybelsus (generic name semaglutide), announced Tuesday it has initiated legal proceedings against some weight loss or wellness clinics, medical spas and compounding pharmacies to combat the sale of compounded versions of their drugs.
Compounding involves combining or changing drugs or ingredients to make a medication designed for a specific patient—in the case of counterfeit Ozempic and Wegovy, the dangerous salt form of semaglutide is used in the injectables, which is different from the approved version of the drug.
Both Ozempic and Wegovy have been on the Food and Drug Administration’s drug shortage list for months following an increase in popularity due to their weight loss benefits.
The FDA issued its own warning about compounded semaglutide in May, stating it’s received reports of adverse events” following the use of compounded versions of the drug, and warned patients shouldn’t use a compounded drug if an approved drug is available.
The FDA also advised patients to proceed with caution, as some of the compounded semaglutide may not have the same active ingredients as the approved version and may contain salt formulations, which are not safe or effective.
Compounded drugs are not FDA-approved- or regulated, so the agency is unable to verify the safety of the medication and they also lack approval of manufacturing quality.
Key Background
The FDA reported it’s previously witnessed “troubling conditions” in some compounded facilities, including pet beds near sterile compounding areas, the use of toaster ovens for sterilization and people handling sterile drug products without skin protection, which can lead to the potential spread of bacteria. Bad compounding practices can cause severe drug quality issues, like contamination, or a drug with too much of an active ingredient. A 2013 study published in Drug R&D found compounded sterile preparations can pose the risk of microbial contamination. Over the course of 11 years, the study reports three separate cases of meningitis outbreaks were linked to “sterile” steroid injections contaminated with either bacteria or fungus made by compounding pharmacies. The U.S. faced its most brutal outbreak involving contaminated compounded drugs in 2012, when a Massachusetts pharmacy shipped drugs contaminated with fungus across the country. These drugs were injected into patients’ spines and joints, resulting in over 750 people in 20 states developing fungal infections, including 60 related deaths. Over 14,000 patients received injections from this batch of contaminated drugs.
Contra
The process of compounding drugs has been used for decades as a remedy for drug shortages. When asthma drug albuterol first went into a shortage earlier this year, hospitals compounded the drug to tailor it to each patient. Compounded drugs are necessary if an FDA-approved drug is unavailable, when a patient needs customized dosing or is allergic to a certain dye and needs the medication to be made without it, according to the Congressional Research Service. However, according to the FDA, this should only be done by practitioners in hospitals, clinics and other health care facilities.
What To Know About Ozempic: The Diabetes Drug Becomes A Viral Weight Loss Hit (Elon Musk Boasts Using It) Creating A Shortage (Forbes)
Wegovy Shortage: Drug Maker Limits Distribution—Here’s When Supplies Should Improve (Forbes)
‘Ozempic Face’ Explained: Why It Happens And How To Fix It (Forbes)
Asthma Drug Albuterol Shortage Is About To Worsen: Here’s Why—And How Hospitals Are Filling The Gaps (Forbes)
Ozempic As A Pill: Drug Makers Race For Cheaper Weight Loss Drugs (Without The Shots) (Forbes)
Read the full article here